As the United States government and medical professionals scope out the manifold effects of the COVID-19 pandemic, one troubling concern stands out among the rest. This concern is for senior citizens, especially those with weaker immune systems. Not only are experts concerned about how susceptible the elderly are to contracting the COVID-19 virus, but also about servicing risks and difficulties. For example, according to the CDC, 25.5% of people under age 65 have public health insurance. Luckily, with the advent of various technological breakthroughs, seniors are not totally out of options.
Seniors and COVID-19
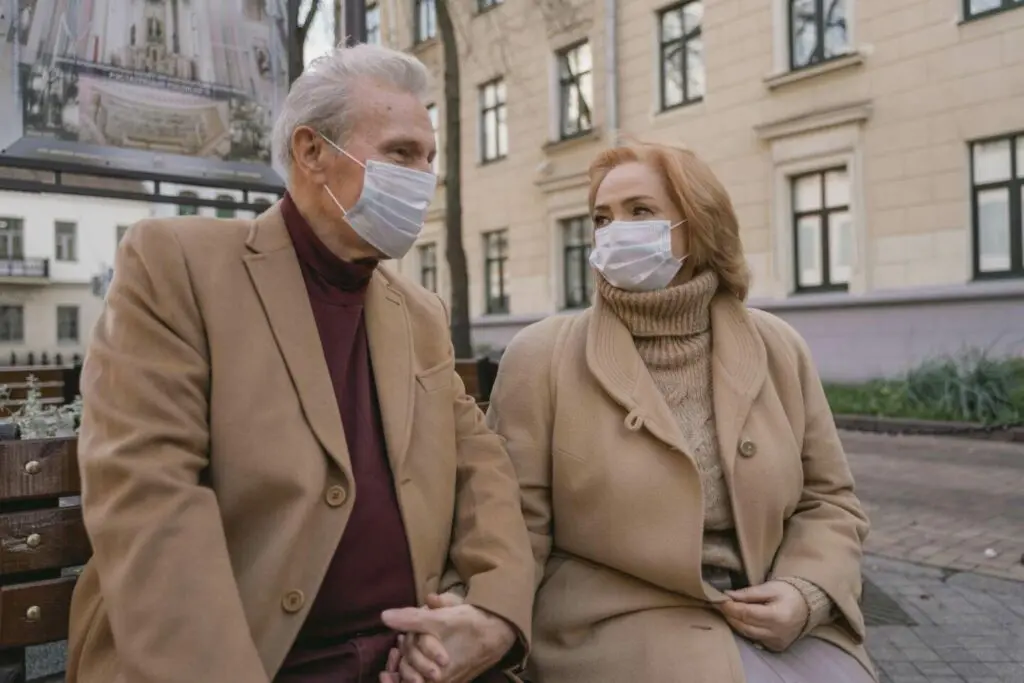
According to the CDC, the COVID-19 risks increase dramatically in correlation to a person’s age. This means that it’s incredibly important for American seniors to comply with CDC guidelines and regulations. Staying indoors as much as possible, wearing a mask in public, and regular hand washing are all essential practices to help the elderly protect themselves from the virus. Nearly 80% of COVID-19 deaths in the USA have been in adults 65 years old or older. It is all the more important, even now, to practice healthy habits to safeguard the vulnerable.
Seniors and Medical Centers
This drastic increase in risk has created a higher demand for hospitalization and emergency care for senior citizens. At the same time, seniors with chronic ailments or other conditions unrelated to COVID-19 put themselves at the risk of exposure when seeking medical attention in medical centers with a high amount of traffic.
Waiting rooms are especially dangerous despite sanitary efforts as other waiting patients could expose elderly citizens to illnesses that further cripple their already vulnerable immune systems. As a result, many seniors have needed to quickly adopt technology and seek care through virtual and remote methods.
Methods of Treatment
The aforementioned dynamic has emphasized the line of demarcation between cases needing regular care, and emergency care for chronic conditions, in order to avoid hospital and on-site visits as much as possible. This means that patients with ailments that are deemed non-urgent by medical staff could have their treatments postponed, which could jeopardize the wellbeing of elderly patients whose ailments affect their motor functions. Luckily, in many instances, healthcare practices have expanded their available array of emergency medical services administered at the patient’s homes. These services range from respiratory issues (such as asthma, bronchitis, or pneumonia) to minor fractures and head injuries.