NATIVE APP
The Future of Health Data Management Is Here
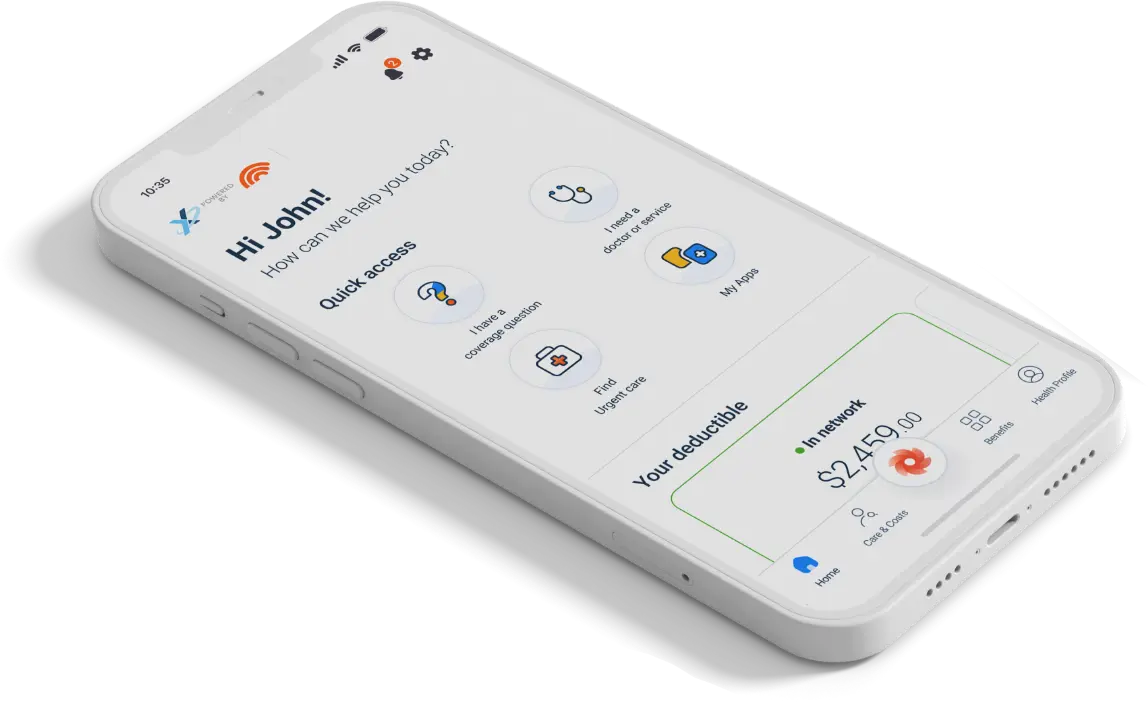
Harnessing the power of AI to maximize benefit utilization and take member engagement to new heights, MediConnX360 2.0, powered by Healthee, simplifies the complexities of health plan navigation, clarifies benefits, and makes accessing care more efficient and affordable.
That means you’re instantly connected – and stay connected – to the industry’s most comprehensive, compliant, and automated claims adjudication and benefits administration solutions.

Discover more
Get Connected Today
To fully see how our system can help you save time, reduce cost, and increase your operation’s compliance, please share your contact information below and we will schedule a confidential demo session.
As the health space and regulations continue to evolve every day, turnkey solutions that are compliant, comprehensive, and future-facing are not only valuable – they’re necessary. MediConnX360 2.0's leading-edge technology and services that provide all the solutions you need today – and tomorrow.
Key Features:
AI-Powered Health Plan Decision-Making Tools:
Participants can compare and share health plan options, allowing for a personalized experience that helps them identify the best plans.
Enhanced Benefits Navigation:
Participants gain clear insights into their benefits, helping them maximize benefit utilization through the Healthee app.
Provider Search & Appointment Scheduling:
Participants can search for in-network providers, view ratings and reviews, and schedule physician, dental, and vision appointments within the app.
Price Transparency Technology:
Participants can see the cost of care in advance for each provider or service, allowing them to choose the most cost-effective care.
Cost-Saving Strategies:
The platform steers participants toward cost-saving strategies, including telehealth services, musculoskeletal (MSK) solutions, and diabetes monitoring.
MediConnX360 2.0, Powered by Healthee, enables administrators to distribute updates, access reports, and offer brokers branded dashboards for streamlined engagement, ensuring full NSA and TiC compliance. Members benefit from easy access to tools for claim verification, enrollment management, and secure communication, making health plan navigation and care coordination more intuitive and efficient.

